There is no permanent cure for SLE. The goal of treatment is to relieve symptoms and protect organs by decreasing inflammation and/or the level of autoimmune activity in the body. Many patients with mild symptoms may need no treatment or only intermittent courses of antiinflammatory medications. Those with more serious illness involving damage to internal organ(s) may require high doses of corticosteroids in combination with other medications that suppress the body's immune system.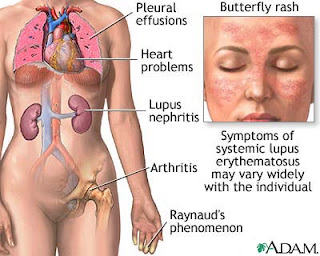 Patients with SLE need more rest during periods of active disease. Researchers have reported that poor sleep quality was a significant factor in developing fatigue in patients with SLE. These reports emphasize the importance for patients and physicians to address sleep quality and the effect of underlying depression, lack of exercise, and self-care coping strategies on overall health. During these periods, carefully prescribed exercise is still important to maintain muscle tone and range of motion in the joints.
Patients with SLE need more rest during periods of active disease. Researchers have reported that poor sleep quality was a significant factor in developing fatigue in patients with SLE. These reports emphasize the importance for patients and physicians to address sleep quality and the effect of underlying depression, lack of exercise, and self-care coping strategies on overall health. During these periods, carefully prescribed exercise is still important to maintain muscle tone and range of motion in the joints.
Nonsteroidal antiinflammatory drugs (NSAIDs) are helpful in reducing inflammation and pain in muscles, joints, and other tissues. Examples of NSAIDs include aspirin, ibuprofen (Motrin), naproxen (Naprosyn), and sulindac (Clinoril). Since the individual response to NSAIDs varies among patients, it is common for a doctor to try different NSAIDs to find the most effective one with the fewest side effects. The most common side effects are stomach upset, abdominal pain, ulcers, and even ulcer bleeding. NSAIDs are usually taken with food to reduce side effects. Sometimes, medications that prevent ulcers while taking NSAIDs, such as misoprostol (Cytotec), are given simultaneously.
Corticosteroids are more potent than NSAIDs in reducing inflammation and restoring function when the disease is active. Corticosteroids are particularly helpful when internal organs are affected. Corticosteroids can be given by mouth, injected directly into the joints and other tissues, or administered intravenously. Unfortunately, corticosteroids have serious side effects when given in high doses over prolonged periods, and the doctor will try to monitor the activity of the disease in order to use the lowest doses that are safe. Side effects of corticosteroids include weight gain, thinning of the bones and skin, infection, diabetes, facial puffiness, cataracts, and death (necrosis) of the tissues in large joints.
Hydroxychloroquine (Plaquenil) is an antimalarial medication found to be particularly effective for SLE patients with fatigue, skin involvement, and joint disease. Consistently taking Plaquenil can prevent flare-ups of lupus. Side effects are uncommon but include diarrhea, upset stomach, and eye-pigment changes. Eye-pigment changes are rare but require monitoring by an ophthalmologist (eye specialist) during treatment with Plaquenil. Researchers have found that Plaquenil significantly decreased the frequency of abnormal blood clots in patients with systemic lupus. Moreover, the effect seemed independent of immune suppression, implying that Plaquenil can directly act to prevent the blood clots. This fascinating study highlights an important reason for patients and doctors to consider Plaquenil for long-term use, especially for those SLE patients who are at some risk for blood clots in veins and arteries, such as those with phospholipid antibodies (cardiolipin antibodies, lupus anticoagulant, and false-positive venereal disease research laboratory test). This means not only that Plaquenil reduces the chance for re-flares of SLE, but it can also be beneficial in thinning the blood to prevent abnormal excessive blood clotting. Plaquenil is commonly used in combination with other treatments for lupus.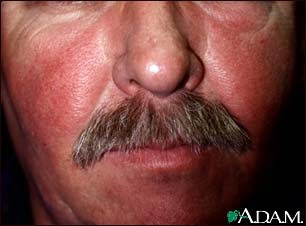 For resistant skin disease, other antimalarial drugs, such as chloroquine (Aralen) or quinacrine, are considered and can be used in combination with hydroxychloroquine. Alternative medications for skin disease include dapsone and retinoic acid (Retin-A). Retin-A is often effective for an uncommon wart-like form of lupus skin disease. For more severe skin disease, immunosuppressive medications are considered as described below.
For resistant skin disease, other antimalarial drugs, such as chloroquine (Aralen) or quinacrine, are considered and can be used in combination with hydroxychloroquine. Alternative medications for skin disease include dapsone and retinoic acid (Retin-A). Retin-A is often effective for an uncommon wart-like form of lupus skin disease. For more severe skin disease, immunosuppressive medications are considered as described below.
Medications that suppress immunity (immunosuppressive medications) are also called cytotoxic drugs. Immunosuppressive medications are used for treating patients with more severe manifestations of SLE, such as damage to internal organ(s). Examples of immunosuppressive medications include methotrexate (Rheumatrex, Trexall), azathioprine (Imuran), cyclophosphamide (Cytoxan), chlorambucil (Leukeran), and cyclosporine (Sandimmune). All immunosuppressive medications can seriously depress blood-cell counts and increase risks of infection and bleeding. Other side effects are specific for each drug. For examples, Rheumatrex can cause liver toxicity, while Sandimmune can impair kidney function.
In recent years, mycophenolate mofetil (Cellcept) has been used as an effective medication for lupus, particularly when it is associated with kidney disease. Cellcept has been helpful in reversing active lupus kidney disease (lupus renal disease) and in maintaining remission after it is established. Its lower side-effect profile has advantage over traditional immune-suppression medications.
In SLE patients with serious brain or kidney disease, plasmapheresis is sometimes used to remove antibodies and other immune substances from the blood to suppress immunity. Rarely, SLE patients can develop seriously low platelet levels, thereby increasing the risk of excessive and spontaneous bleeding. Since the spleen is believed to be the major site of platelet destruction, surgical removal of the spleen is sometimes performed to improve platelet levels. Other treatments have included plasmapheresis and the use of male hormones. Plasmapheresis has also been used to remove proteins (cryoglobulins) that can lead to vasculitis. End-stage kidney damage from SLE requires dialysis and/or a kidney transplant.
Most recent research is indicating benefits of rituximab (Rituxan) in treating lupus. Rituximab is an intravenously infused antibody that suppresses a particular white blood cell, the B cell, by decreasing their number in the circulation. B cells have been found to play a central role in lupus activity, and when they are suppressed, the disease tends toward remission. This may particularly helpful for patients with kidney disease.
At the 2007 national Rheumatology meeting, there was a paper presented suggesting that low-dose dietary supplementation with omega-3 fish oils could help patients with lupus by decreasing disease activity and possibly decreasing heart-disease risk.
Image Source
February 3, 2009
Treatment Systemic lupus erythematosus / Lupus
Posted at 11:45 PM 0 comments
What Is Systemic lupus erythematosus / SLE / Lupus ?
Lupus is an autoimmune disease characterized by acute and chronic inflammation of various tissues of the body. Autoimmune diseases are illnesses that occur when the body's tissues are attacked by its own immune system. The immune system is a complex system within the body that is designed to fight infectious agents, such as bacteria and other foreign microbes. One of the ways that the immune system fights infections is by producing antibodies that bind to the microbes. Patients with lupus produce abnormal antibodies in their blood that target tissues within their own body rather than foreign infectious agents.  Because the antibodies and accompanying cells of inflammation can affect tissues anywhere in the body, lupus has the potential to affect a variety of areas. Sometimes lupus can cause disease of the skin, heart, lungs, kidneys, joints, and/or nervous system. When only the skin is involved, the condition is called lupus dermatitis or cutaneous lupus erythematosus. A form of lupus dermatitis that can be isolated to the skin, without internal disease, is called discoid lupus. When internal organs are involved, the condition is referred to as systemic lupus erythematosus (SLE).
Because the antibodies and accompanying cells of inflammation can affect tissues anywhere in the body, lupus has the potential to affect a variety of areas. Sometimes lupus can cause disease of the skin, heart, lungs, kidneys, joints, and/or nervous system. When only the skin is involved, the condition is called lupus dermatitis or cutaneous lupus erythematosus. A form of lupus dermatitis that can be isolated to the skin, without internal disease, is called discoid lupus. When internal organs are involved, the condition is referred to as systemic lupus erythematosus (SLE).
Both discoid and systemic lupus are more common in women than men (about eight times more common). The disease can affect all ages but most commonly begins from 20 to 45 years of age. Statistics demonstrate that lupus is somewhat more frequent in African Americans and people of Chinese and Japanese descent.
What are the symptoms and signs of lupus?
Patients with SLE can develop different combinations of symptoms and organ involvement. Common complaints and symptoms include fatigue, low-grade fever, loss of appetite, muscle aches, arthritis, ulcers of the mouth and nose, facial rash ("butterfly rash"), unusual sensitivity to sunlight (photosensitivity), inflammation of the lining that surrounds the lungs (pleuritis) and the heart (pericarditis), and poor circulation to the fingers and toes with cold exposure (Raynaud's phenomenon). Complications of organ involvement can lead to further symptoms that depend on the organ affected and severity of the disease.
Skin manifestations are frequent in lupus and can sometimes lead to scarring. In discoid lupus, only the skin is typically involved. The skin rash in discoid lupus often is found on the face and scalp. It usually is red and may have raised borders. Discoid lupus rashes are usually painless and do not itch, but scarring can cause permanent hair loss. Over time, 5%-10% of patients with discoid lupus may develop SLE.
Over half of the patients with SLE develop a characteristic red, flat facial rash over the bridge of their nose. Because of its shape, it is frequently referred to as the "butterfly rash" of SLE. The rash is painless and does not itch. The facial rash, along with inflammation in other organs, can be precipitated or worsened by exposure to sunlight, a condition called photosensitivity. This photosensitivity can be accompanied by worsening of inflammation throughout the body, called a "flare" of the disease.
Typically, this rash can heal without permanent scarring with treatment.
Most patients with SLE will develop arthritis during the course of their illness. Arthritis in SLE commonly involves swelling, pain, stiffness, and even deformity of the small joints of the hands, wrists, and feet. Sometimes, the arthritis of SLE can mimic that of rheumatoid arthritis (another autoimmune disease).
More serious organ involvement with inflammation occurs in the brain, liver, and kidneys. White blood cells and blood-clotting factors also can be characteristically decreased in SLE, known as leucopenia and thrombocytopenia, respectively. Leucopenia can increase the risk of infection and thrombocytopenia can increase the risk of bleeding.
Inflammation of muscles (myositis) can cause muscle pain and weakness. This can lead to elevations of muscle enzyme levels in the blood.
Inflammation of blood vessels (vasculitis) that supply oxygen to tissues can cause isolated injury to a nerve, the skin, or an internal organ. The blood vessels are composed of arteries that pass oxygen-rich blood to the tissues of the body and veins that return oxygen-depleted blood from the tissues to the lungs. Vasculitis is characterized by inflammation with damage to the walls of various blood vessels. The damage blocks the circulation of blood through the vessels and can cause injury to the tissues that are supplied with oxygen by these vessels.
Inflammation of the lining of the lungs (pleuritis) and of the heart (pericarditis) can cause sharp chest pain. The chest pain is aggravated by coughing, deep breathing, and certain changes in body position. The heart muscle itself rarely can become inflamed (carditis). It has also been shown that young women with SLE have a significantly increased risk of heart attacks from coronary artery disease.
Kidney inflammation in SLE can cause leakage of protein into the urine, fluid retention, high blood pressure, and even kidney failure. This can lead to further fatigue and swelling of the legs and feet. With kidney failure, machines are needed to cleanse the blood of accumulated poisons in a process called dialysis.
Involvement of the brain can cause personality changes, thought disorders (psychosis), seizures, and even coma. Damage to nerves can cause numbness, tingling, and weakness of the involved body parts or extremities. Brain involvement is referred to as lupus cerebritis.
Many patients with SLE experience hair loss (alopecia). Often, this occurs simultaneously with an increase in the activity of their disease. The hair loss can be patchy or diffuse and appear to be more like hair thinning.
Some patients with SLE have Raynaud's phenomenon. In these patients, the blood supply to the fingers and/or toes becomes compromised upon exposure to cold, causing blanching, whitish and/or bluish discoloration, and pain and numbness in the exposed fingers and toes.
Image Source
Posted at 11:28 PM 0 comments
What Is Koilonychia ?
Koilonychia is a nail disorder that affects the color, shape, texture, and thickness of your fingernails or toenails and often associated with iron-deficiency with or without anemia. Know more about it-causes, symptoms, prevention and treatment in the following article.
Koilonychia literally means ‘spoon nails.’ It refers to nails that become flat, lose their convex contour and replaced by a central concave contour with raised edges, and lose their natural color. The nail usually becomes thin and brittle.
Causes
* It is often associated with iron-deficiency with or without anemia.
* It can be linked to other causes such as thyroid dysfunction, renal disease, impaired peripheral circulation, systemic lupus erythematosus, Hypoplastic Patella musculoskeletal conditions, hemochromatosis, Raynaud's Disease, nail-patella syndrome and Hypoplastic Patella.
* It may result from trauma.
* Malnutrition
* Injury of nail plate
* Constant occupational exposure of hand nails to petroleum, diesel and other petroleum based products and solvents
* Excessive use of oils and soaps
Prevention
If you observe Koilonychia, immediately take the following preventive measures and you can easily avoid it, before it becomes serious.
* Avoid using your nails as tools to pick, poke or pry things.
* Wear gloves while washing dishes and handling detergents and chemicals.
* Avoid biting your nails.
* Avoid wearing shoes that are tight around the toes.
* Avoid exposure to nail polish and moisture for a long time.
Treatment and Natural Home Remedies for Koilonychia
Koilonychia should be treated as soon as it is recognized.
* The first step of treating koilonychia includes consulting a specialist and following the treatments and suggestions accordingly.
* Since it is associated with iron deficiency, take iron based foods and essential vitamins. However be sure to take the required iron and avoid mixing it with beverages such as tea or coffee as they inhibit iron absorption.
* Using an emollient intended especially for the nails right after a shower or washing hands will keep the nails nourished and Koilonychia at bay.
Image Source
Posted at 11:20 PM 0 comments
What Is Alopecia areata ?
Alopecia areata is a hair-loss condition which usually affects the scalp. It can, however, sometimes affect other areas of the body. Hair loss tends to be rather rapid and often involves one side of the head more than the other.
Alopecia areata affects both males and females. This type of hair loss is different than male-pattern baldness, an inherited condition.
What causes alopecia areata?
Current evidence suggests that alopecia areata is caused by an abnormality in the immune system. This particular abnormality leads to autoimmunity. As a result, the immune system attacks particular tissues of the body. In alopecia areata, for unknown reasons, the body's own immune system attacks the hair follicles and disrupts normal hair formation. Biopsies of affected skin show immune cells inside of the hair follicles where they are not normally present. What causes this is unknown. Alopecia areata is sometimes associated with other autoimmune conditions such as allergic disorders, thyroid disease, vitiligo, lupus, rheumatoid arthritis, and ulcerative colitis. Sometimes, alopecia areata occurs within family members, suggesting a role of genes and heredity.
What causes this is unknown. Alopecia areata is sometimes associated with other autoimmune conditions such as allergic disorders, thyroid disease, vitiligo, lupus, rheumatoid arthritis, and ulcerative colitis. Sometimes, alopecia areata occurs within family members, suggesting a role of genes and heredity.
How is alopecia areata diagnosed?
The characteristic finding of alopecia areata is the exclamation point hair. These unusual hairs can be found in areas of hair loss. They are visible with a hand lens as short, broken off hairs that are narrower closer to the scalp (appearing like an exclamation point). A biopsy of the scalp is sometimes necessary for a diagnosis.
How is alopecia areata treated?
In approximately 50% of patients, hair will regrow within a year without any treatment. The longer the period of time of hair loss, the less likelihood that the hair will regrow. A variety of treatments can be tried. Steroid injections, creams, and shampoos (such as clobetasol or fluocinonide) for the scalp have been used for many years. Other medications include minoxidil, irritants (anthralin or topical coal tar), and topical immunotherapy (cyclosporine), each of which are sometimes used in different combinations.
A study reported in the journal Archives of Dermatology (vol. 134, 1998;1349-52) showed effectiveness of aromatherapy essential oils (cedarwood, lavender, thyme, and rosemary oils) in some patients. As with many chronic disorders for which there is no single treatment, a variety of remedies are promoted which in fact have no benefit. There is no known effective method of prevention, although the elimination of emotional stress is felt to be helpful. No drugs or hair-care products have been associated with the onset of alopecia areata. Much research remains to be completed on this complex condition.
Image Source
Posted at 11:08 PM 0 comments
What Is Acne Fulminans ?.
Acne fulminans is a rare and very severe form of acne conglobata associated with systemic symptoms. It nearly always affects males.
It is characterised by: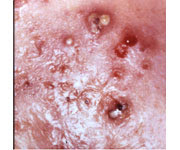 * Abrupt onset
* Abrupt onset
* Inflammatory and ulcerated nodular acne on chest and back
* Severe acne scarring
* Fluctuating fever
* Painful joints
* Malaise (ie. the patient feels unwell)
* Loss of appetite and weight loss
* Raised white blood cell count.
Although it mostly just happens, it may be precipitated by:
* Testosterone (legally prescribed or illegally taken to enhance muscle growth)
* Isotretinoin
The syndrome SAPHO (Synovitis, Acne, Pustulosis, Hyperostosis and Osteitis) may be a serious complication of acne fulminans.
Management.
Patients with acne fulminans should consult a dermatologist urgently. Management can prove difficult, and several medications are usually required. These may include:
* High doses of oral antibiotics such as erythromycin (2g/day)
* Anti-inflammatory medications such as salicylates (aspirin)
* Systemic oral steroids such as prednisone (20-60mg/day)
* Dapsone
* Isotretinoin
Topical acne medications are unhelpful.
Image
Source
Posted at 10:57 PM 0 comments
What Is Acne Cosmetica?
Acne cosmetica is a mild but persistent form of acne. As the name implies, acne cosmetica is triggered by the use of cosmetics. It can occur anywhere on the body, but is much more common on the face, neck, hairline and scalp.
What Does Acne Cosmetica Look Like?
Acne cosmetica looks like small bumps across the surface of the skin or scalp. The skin will look and feel rough. Many comedones, and possibly some small papules and pustules, will be present. There is little to no inflammation.
What Causes Acne Cosmetica?
This type of acne is caused by the use of comedogenic hair or skin care products. When a cosmetic product accumulates within the follicle, the pore becomes blocked. Excess skin oil builds up, clogging the pore and creating a blemish.
Pomades or hair oils, heavy moisturizers, eye creams, and makeup are all common causes of acne cosmetica.
* Is My Makeup Causing Pimples?
How Can Acne Cosmetica Be Treated?
Identifying the pore-clogging culprit is important. Are you breaking out on the forehead, hairline or scalp? Your hair care products may be to blame. Finding small bumps and whiteheads in the eye area or on the upper cheeks? Your eye cream could be too heavy. Bumpiness and breakouts over the entire face and neck area most likely are caused by moisturizer or foundation makeup. Once the source of the breakouts is identified and use is discontinued, acne cosmetica gradually improves.
Sometimes it's not practical to stop using your hair or skin care products. You can still reduce the amount of pore blockages produced by only choosing products labeled "noncomedogenic". Switch to an oil-free moisturizer. Apply hair pomades and oils at least one inch back from the hairline, or only on the ends of the hair, if possible. And make sure to thoroughly cleanse all traces of makeup from your face at the end of each day.
To help clear existing breakouts more quickly, and to inhibit the formation of new comedones, use a cleanser or treatment pads containing salicylic acid. Regular exfoliation may also help to speed clearing of acne cosmetica. As with any form of acne, see your doctor if you aren't seeing improvement after six to eight weeks of treatment.
Source
Posted at 10:38 PM 0 comments

